A 60yo black male came in for a two month follow up after his comprehensive exam to repeat his visual field and check his IOP. Systemically, he is being treated for type 2 DM, sleep apnea, and POAG. His current medications include aspirin, Farxiga, metformin, pravastatin, Latanoprost and Cosopt.
His incoming vision is 20/20 in each eye and pupils and EOMs are normal in both eyes.
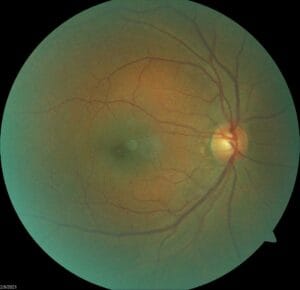
He has some mild nuclear cataracts as the only significant anterior segment finding. IOPs are 24/24 at 11:30 AM at this visit. Small pupil exam shows no evidence of drance hemorrhages and otherwise looks stable to previous photos as seen below.

His latest visual field is shown next.


There is no change compared to baseline field taken in 2018.
Other test findings include pachymetry of 514/526 and open gonioscopy both eyes. An RNFL OCT shows OD borderline thinning superior and OS thinning superior-temporally.
Prior to treatment, his max IOP was 25/25. The patient was treated with Latanoprost only for two years and during that time, IOPs ranged from 16-22 OD, 15-22 OS. Cosopt was added and IOPs have continued to range from 20-24 in both eyes in the last two years.
The patient admits to often missing his eyedrops a few times each week.
Given the lack of adequate IOP reduction but otherwise stable OCT and visual fields in this patient’s case, what would you do next? How would you classify this patient’s POAG? What are your comments on the visual fields?