A 69 year old patient was coming in for her 6 month follow up for moderate NPDR OU. She reports that there has been no vision or other ocular changes since the last visit.
Systemically, she has DM2 with a latest HbA1C of 8.1 from March, HTN, hepatitis B, psoriasis, stage 4 chronic kidney disease, hyperlipidemia, GERD, and liver cirrhosis. She is taking a lot of medications including atorvastatin, entecavir, furosemide, insulin, labetalol, and semaglutide with reported good compliance.
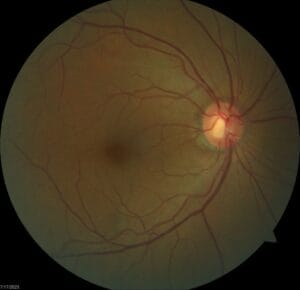
She came to the exam uncorrected with a VA of OD 20/70, OS 20/40, pinhole to OD 20/50 and no improvement in OS.
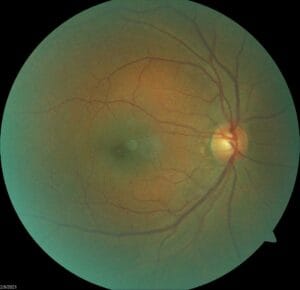
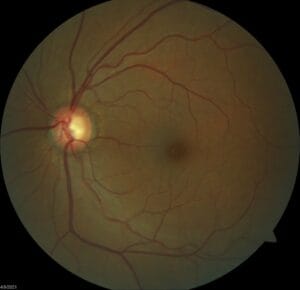
Anterior segment is stable to previous visits with clear PC-IOLs. Posterior segment shows stable moderate NPDR both eyes.
This doesn’t sound like anything unusual for this patient, we’d been monitoring her every six months for moderate NPDR since she first came to us in 2021. So why am I writing about her now?
For each of her prior visits, she had been able to see 20/25 or 20/30 with correction or pinhole. This was a change and decrease in vision, even though the patient herself had not noticed.
I get it. In a busy and crazy clinic like the community clinic I am in, it’s easy to just follow the plan and call it a day. But when something is different, it warrants digging a little deeper. So I had the student build the trial frame for this patient based on the prescription we found in January and her vision still did not improve.
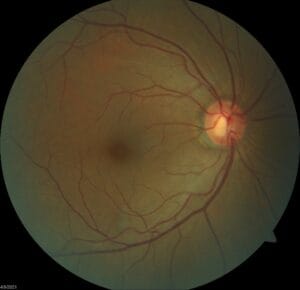
The student was concerned that some of the hard exudates we saw were approaching the foveas and could be causing some macular edema so we took an updated OCT. At first glance, the student said everything looked fine. All retinal layers were intact and there was actually no evidence of macular edema. So if there wasn’t any edema and her refraction did not improve anything, why did this patient have reduced visual acuity?
Thankfully, when we looked at the OCT a little closer, we noticed actually a fair amount of vitreomacular traction in both eyes, enough to cause a little bit of distortion to the retinal layers, although she was correct, everything was still intact.
Now I felt a little better having a reason for this patient’s change in vision, but it got the student and I to have a conversation about how putting all this information together was important in helping us determine how to manage the patient moving forward. Did we need to refer her out to retina or could we still see her? Did we need to modify our follow up plan?
We opted to follow her a little more closely than 6 months and we’ll see how it goes from there.
Are there any takeaways or other points of discussion from you at this point? I’m always interested.