Today’s case is a short one. The patient is a 38 year old Hispanic female who was last seen a year and a half ago for a diabetes eye exam. She had been correctable to 20/20-3 and 20/20-1 with a refraction of OD +0.25-2.00×005, OS plano DS. She comes in today saying she has blurred distance vision especially when driving at night and that she never filled the glasses prescription from last year and has never worn glasses ever.
As I mentioned, she has had diabetes since about 2003 with a latest HbA1c of 10.1 from 3 months ago. She also has diagnoses of anxiety and depression, migraine, vertigo, gastritis, and reports quitting smoking about 3 weeks prior. Her medications include albuterol, zyrtec and flonase, glipizide, metformin, and protonix. She has an allergy to eletriptan (she gets hives).
Confrontation testing of pupils, EOMs, visual fields are all normal. Incoming uncorrected visual acuity is OD 20/50-2, OS 20/25-2.
Retinoscopy shows OD plano -2.00 x 180, OS plano -0.50 x 180
Refraction shows OD -0.75 -1.25 x 175 20/25, OS -0.50 DS 20/25+2
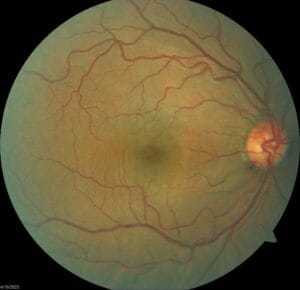
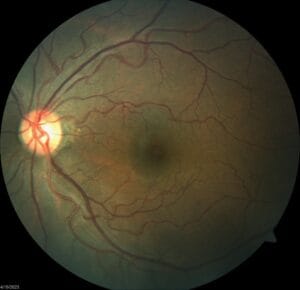
Anterior segment shows some mild punctate erosions inferiorly of both eyes and is otherwise clear with IOPs of 13/13 mm Hg. Posterior segment of both eyes is clear of any pathology or DM retinopathy.
What would you prescribe for this patient? Do her visual acuities match her refraction results?
She had a myopic shift in her eyes compared to her last exam 1.5 years ago. Are you more or less willing to prescribe her glasses because of this shift?
The patient also reports her history of vertigo. Does this mean you should modify her prescription in any way? Considering she’s also never worn glasses in the past, would you modify her prescription any differently?
Let me know your thoughts!