My attending doctor the summer of my third year asked us to guess our patients’ glasses prescriptions each time we walked them back to our room. There were no prizes or incentives for us to guess ‘right’, but what inadvertently happened was that started a path of guessing every part of the exam moving forward.
Sure, it’s one thing to peek at a person’s glasses when you first introduce yourself – obviously myopic lenses will look different from hyperopic lenses. And based on the patient’s age, I could guess if a patient was wearing progressives or not before I neutralized their prescription. I would guess the patient’s add if they were in a multi-focal design.
Taking that guessing game into the rest of the exam though, that was where the fun started and I believe that’s what helped me grow as a clinician. I was always anticipating what the next result would be and that kept me curious. Depending on the answers I got, that helped refine which way an exam would go.
Let’s say a middle-aged patient came in and off the bat says they can’t see well out of one eye. Immediately, I’ve broken things down categorically – can this be a refractive issue, a binocular vision issue, or related to some kind of ocular pathology? What question or set of questions can I ask to help me focus on a likely differential within the first few minutes of the exam?
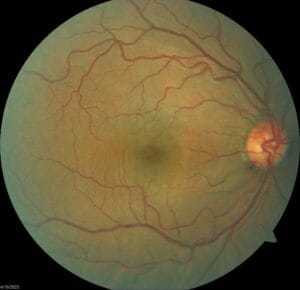
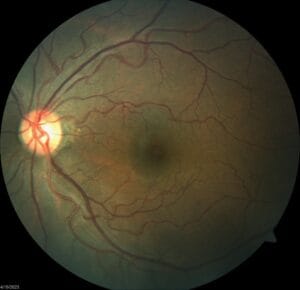
Let’s say you go through your confrontation testing and the right eye is light perception and the left eye is a soft 20/20- without correction. EOMs are full but you notice a mild RAPD in the right eye. Also, when you’re doing pupil testing, you notice something white where the lens should be – the other eye seems clear. Confrontation fields are full for the left eye but he is unable to distinguish anything besides light in the right eye.
At this point, you probably have ruled out refractive error and binocular vision as a top differential to this patient’s poor vision. With that in mind, you should know anticipate that refraction really shouldn’t take you very long – big steps are likely not going to help the right eye and you should already guess that the left eye will have a very minimal prescription at all. Recommending an age appropriate add is likely okay here but your goal here was to get to dilation as quickly as possible to fully assess the patient’s ocular health.
As you’re dilating the patient, what can you anticipate about this patient’s ocular health? Does a white cataract account for light perception vision? What could have contributed to this patient’s cataract development in the right eye? Would you anticipate any lenticular changes in the left eye? What are some causes of asymmetric lens changes, especially if the patient (including this one) strongly denies any history of ocular trauma?
Take a different patient now who was last seen two years ago, was correctable to 20/20- in both eyes but already showed evidence of moderate nonproliferative diabetic retinopathy OU. If this patient came in and saw you today saying his vision in the right eye has been bad for the last year, what would you expect? There could be a refractive shift, sure, but less likely if it was only monocular. If I told you he came in needing extra help with walking because he had his left foot amputated from diabetic complications in the last couple months, what would you expect to see in terms of this patient’s ocular health?
Predicting what you’re going to find can help you decide if you need to spend time doing a thorough, careful refraction or performing different binocular vision tests or going straight to ocular health. You can also anticipate your patients’ concerns – is their vision going to get better, are they going to need a referral for surgery or other specialty care, are there any supplements or exercises that you’d recommend for their condition, etc.
Approaching exams this way has kept a lot of exams from feeling too ‘routine’, especially if I can force myself to give at least two two three differentials for whatever it is I’m finding. Besides, who can resist having fun in the exam room even if it’s a game you’re playing by yourself and no one else has to know?
Happy guessing!